Introduction
Cancer is a leading cause of death in Wisconsin, with nearly 12,000 deaths and more than 30,000 new diagnoses each year.
The burden of cancer remains vast, taking a physical, emotional, social, and financial toll on patients, families, caregivers, and communities. Unfortunately, some of our communities are burdened far more than others.
Every Wisconsinite should have the ability to reduce their cancer risk, receive timely diagnosis of and quality treatment for cancer, and enjoy the highest possible quality of life beyond a cancer diagnosis.
The Wisconsin Cancer Plan 2020-2030 lays forth a blueprint for action with a singular vision: creating a healthier Wisconsin by reducing the burden of cancer for everyone. It spans the entire cancer control continuum, from risk reduction through end of life. The success of the Wisconsin Cancer Plan depends on people and organizations from multiple sectors coming together to take action.
Vision
A healthier Wisconsin by reducing the burden of cancer for everyone.
Mission
To engage partners to develop, promote, and implement a statewide comprehensive approach to cancer control.
Overarching goals
- Advance health equity as it relates to cancer.
- Reduce the risk of developing cancer.
- Detect cancer at the earliest stage possible.
- Reduce death and suffering from cancer.
- Improve the quality of life for cancer survivors.
- Improve the quality and use of cancer-related data.
Using the Wisconsin Cancer Plan 2020-2030 to take action
Organizations can look to the Wisconsin Cancer Plan 2020-2030 for evidence-based, sustainable solutions to reduce the burden of cancer in their communities and across the state, through policy and systems-level change.
The Wisconsin Cancer Plan 2020-2030 includes a framework that encompasses the vision, mission, and overarching goals across seven chapters. Each chapter includes priorities, strategies, and specific action steps. To allow for routine revisions, action steps are available only in the online version of the Wisconsin Cancer Plan 2020-2030.
How the Wisconsin Cancer Plan 2020-2030 was developed
The Wisconsin Cancer Plan 2020-2030 was developed by the Wisconsin Cancer Collaborative, a statewide coalition of more than 140 organizations. Over the course of 18 months, a 20-person Steering Committee, representing multiple sectors and organization types, established a framework and guided a process to gather input from stakeholders across the state. Stakeholders were convened twice in-person between June and October 2019 to review evidence and share ideas. Input was reviewed, summarized, and incorporated by staff, stakeholders, and Steering Committee members between October 2019 and May 2020.
The Wisconsin Cancer Plan 2020-2030 will be maintained and updated by the Wisconsin Cancer Collaborative’s Steering Committee and members. Changes based on evolving evidence and emerging needs can be requested here. Requests will be reviewed quarterly by the Wisconsin Cancer Collaborative’s Steering Committee. A review of data and progress toward goals will be routinely reported to members and will be used to determine any needed revisions.
Suggested citation: Wisconsin Cancer Plan 2020-2030. Madison, WI: University of Wisconsin Carbone Cancer Center and Wisconsin Department of Health Services; 2020. Available online at: www.wicancer.org.
Chapter 1
Health Equity
Chapter 1 Overview

Select a priority to learn more
- Priority 1 Increase capacity to reduce the burden of cancer for everyone.
- Priority 2 Increase the number of Wisconsinites with access to quality health care.
- Priority 3 Increase and prioritize health improvement approaches that engage, center, and benefit populations and communities at highest risk of health-related inequities.
Everyone in Wisconsin deserves the chance to live life to the fullest.
This means having the resources needed to make healthy choices and receiving the highest quality care.
In Wisconsin today, some populations are more likely to develop cancer and die from cancer. Social and economic factors, as well as our physical environment, contribute to our overall health. Where people are born, live, work, worship, learn, play, and age—otherwise known as the social determinants of health—can make it more or less challenging to access quality health care and engage in healthier behaviors, which largely determine the quality and length of one’s life.
We can ensure everyone has the chance to live life to the fullest when we:
- Increase our state’s capacity to reduce the burden of cancer for everyone.
- Increase the number of Wisconsinites who have access to quality health care that is both culturally and linguistically appropriate.
- Prioritize activities that engage, center, and benefit populations at higher risk of health-related inequities.
- Commit organizational energy to addressing social determinants of health.
The Takeaway
We will improve health outcomes for everyone in Wisconsin when we improve the conditions in which people are born, live, work, worship, learn, play, and age. By incorporating opportunities for every person attain their full health potential into cancer control efforts, we can reduce the unequal burden of cancer in Wisconsin.
Key Terms
Health equity: A condition achieved when every person has the opportunity to “attain their full health potential” and no one is “disadvantaged from achieving this potential because of social position or other socially determined circumstances.”2
Health inequity: Preventable and unjust differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations.3
Social determinants of health: Conditions in the environment in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.4
Trauma-informed care: An approach to engaging people with histories of trauma that recognizes the presence of trauma symptoms and acknowledges the role that trauma has played in their lives.5
- Other approaches such as healing-centered engagement are beginning to positively reframe trauma by focusing on resilience and collective strength.
References:
- University of Wisconsin Population Health Institute. (2019). County Health Rankings & Roadmaps 2019. Retrieved from :www.countyhealthrankings.org
- Centers for Disease Control and Prevention. (2020, March 11). National Centers for Disease Control and Prevention and Health Promotion. Retrieved from Health Equity: https://www.cdc.gov/chronicdisease/healthequity/index.htm
- Centers for Disease Control and Prevention. (2008). Community Health and Program Services (CHAPS): Health Disparities among Racial/Ethnic Populations. Atlanta: U.S. Department of Health and Human Services
- Centers for Disease Control and Prevention. (2018, January 29). Social Determinants of Health: Know What Affects Health. Retrieved from: https://www.cdc.gov/socialdeterminants/index.htm
- Wisconsin Department of Health. (2020, April 10). Prevention and Healthy Living. Retrieved from Resilient Wisconsin: https//www.dhs.wisconsin.gov/tic/index.htm
Priority 1: Increase capacity to reduce the burden of cancer for everyone.
Strategy A: Increase the diversity and engagement of the Wisconsin Cancer Collaborative membership and partners.
Action Steps
- Evaluate current membership to assure all communities and sectors are represented.
- Actively recruit members that represent different backgrounds and viewpoints.
- Increase the engagement of underrepresented individuals and organizations in the development and implementation of cancer control activities.
- Engage non-traditional partners, including but not limited to: employers, for-profit organizations, faith-based communities, and behavioral health organizations.
- Create environments that will allow the greatest representation of people and organizations to participate.
Strategy B: Increase trust between communities and those working to reduce the burden of cancer.
Action Steps
- Acknowledge factors that have contributed to distrust and work to rebuild trust.
- Engage and center communities at highest risk of health-related inequities when working on health improvement activities.
- Use evidence-based strategies and activities to reduce bias, discrimination, and racism within public health and health care systems.
- Address social determinants of health in the development and evaluation of projects and programs.
- Provide culturally appropriate services and education aimed at populations disproportionally impacted by cancer burdens.
- Adopt organization-wide trauma-informed care policies, practices, and procedures that screen for trauma.
- Train staff in trauma-specific treatment approaches.
Strategy C: Establish and maintain a diverse workforce of health professionals and researchers that better represents all Wisconsin communities.
Action Steps
- Increase K-12 health profession pipeline programs and participation in areas with underrepresented students.
- Establish mentorship opportunities to match underrepresented health professionals and researchers with underrepresented students and trainees.
- Improve cultural competency and the varied representation of the health workforce.
- Increase underrepresented graduates from health profession higher education programs.
- Support professional development opportunities for underrepresented executive and mid-level leaders.
- Support fulfillment and job satisfaction strategies to prevent turnover.
- Increase retention of underrepresented health professionals and researchers.
- Increase health profession and research training opportunities for community members.
- Employ health professionals and researchers from the community in which they serve.
Priority 2: Increase the number of Wisconsinites with access to quality health care.
Strategy A: Increase availability of and access to health services for the under- and uninsured.
Action Steps
- Sustain and promote Wisconsin Well Woman Program and Well Woman Medicaid.
- Support certification of Federally Qualified Health Centers (FQHCs).
- Sustain Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs), and Indian Health Service Health Facilities by expanding capacity and funding support.
- Maintain funding for Vaccines for Children (VFC) program to provide no-cost vaccinations to Medicaid eligible, underinsured, uninsured, and American Indian/Alaskan Native children.
- Aid Federally Qualified Health Centers (FQHCs) in writing federal operating grants.
- Support the adoption of health information technology and technical assistance in Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs).
- Support coverage of secure telehealth services.
- Educate policymakers on the need for universal access to broadband for patients to participate in telehealth services.
- Increase collaboration with Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs).
- Provide transportation services and support for patients to access safety-net health services.
- Increase access and funding for recommended cancer screenings among rural and populations experiencing cancer disparities.
- Provide community opportunities to access low-cost or free early detection cancer screenings.
- Educate policymakers on evidence-based policies that increase access to health services for under- and uninsured.
- Establish and maintain health services within the community to minimize travel and barriers to access.
- Increase the availability of extended clinic hours.
- Increase the number of Wisconsinites with a medical home.
- Educate decision-makers on evidence-based policies that encourage organizations to pay their employees living wages, provide health insurance and paid sick leave.
- Establish a plan to provide equitable access to health services for those under- and uninsured during public health emergencies.
Strategy B: Increase availability of and access to comprehensive health insurance coverage.
Action Steps
- Increase access to Medicaid for uninsured adults and children.
- Increase reimbursement rates under Medicaid.
- Increase access to affordable public and private insurance plans.
- Increase the availability of financial navigators to help enroll community members and answer questions.
- Increase insurance coverage and reimbursement of patient navigators, community health workers, and other support services.
- Eliminate insurance loopholes that limit an individual’s ability to obtain medically necessary prevention, genetic counseling, screening, treatment, and survivorship services.
- Ensure protection for pre-existing conditions are maintained.
- Ensure protections against lifetime limits are maintained.
- Increase the portability of insurance coverage to eliminate gaps in coverage due to transitions in employment or life circumstances.
- Define the essential health benefits that qualified health plans must provide and ensure that these benefits affordably align with Wisconsinites’ needs.
- Increase access to and use of evidence-based preventive services.
Priority 3: Increase and prioritize health improvement approaches that engage, center, and benefit populations and communities at highest risk of health-related inequities.
Strategy A: Collect, examine, and disseminate data on traditionally underrepresented populations.
Action Steps
- Identify existing data sources and collect missing data to examine and monitor trends within and across underrepresented populations.
- Expand existing database and tracking systems to include factors that impact health for all.
- Engage members within underrepresented populations to lead and/or advise data collection and dissemination products.
- Assess rural-urban cancer rates in Wisconsin and develop and implement rural-focused cancer control strategies in areas with high rural cancer incidence and mortality rates.
- Track populations with the highest cancer morbidity and mortality rates.
Strategy B: Increase funding opportunities that address health-related inequities.
Action Steps
- Track and monitor funding opportunities for community-led solutions.
- Include community-based programs in the development of funding opportunities.
- Increase community capacity to shape outcomes, identify funding opportunities, and receive funding.
- Reduce the burden of funding reporting requirements by partnering with community members to develop a shared vision and work together to shape outcomes.
- Increase funding opportunities for community-led programs with relevant and realistic expectations built on trust and community expertise.
- Identify and fund a variety of partner organizations to conduct community-based participatory research.
- Broadly disseminate information and support for funding opportunities.
Strategy C: Increase the co-development of health improvement activities with and for populations at highest risk of health-related inequities.
Action Steps
- Value community knowledge and experience by incorporating practice-based evidence and promising practice.
- Increase representation and engagement of communities in the development and implementation of cancer control activities.
- Increase awareness among the public and health providers about the social determinants of health and their influence on cancer rates.
- Identify and engage with populations with the highest cancer morbidity and mortality rates.
- Conduct community-based participatory research to establish evidence-based interventions and promising practices that address the social determinants of health in communities.
Strategy D: Increase policy and systems-level changes that address the social determinants of health.
Action Steps
- Increase awareness among the public and health providers about the social determinants of health and their influence on cancer rates.
- Identify gaps in knowledge and awareness of the connection between the social determinants of health and the burden of cancer.
- Incorporate and address social determinants of health in community health improvement plans.
- Establish a standard social determinants of health screening tool and include it in electronic health records.
- Incorporate the social determinants of health into research activities.
- Train all staff on the social determinants of health and evidence-based practices to address social determinants of health within their role and organization.
- Create and maintain resources that mitigate social determinants of health, such as housing access and transportation solutions.
- Adopt a “health in all policies” approach (a collaborative approach that integrates health considerations into policymaking across sectors) to address health in all areas of social, economic, and health policies.
- Invest time and financial resources to equitably improve Wisconsin’s economic and education systems.
- Educate decision-makers on evidence-based policies that improve population health and well-being by providing a living wage.
- Adopt institutional policies that pay employees a living wage with benefits, including comprehensive health insurance.
- Invest in organizations, projects, and programs that have policies to pay employees a living wage with benefits, including comprehensive health insurance.
- Educate decision-makers on the health impacts of employment requirements for essential health services, particularly for those suffering and unable to work due to a cancer diagnosis.
- Invest in education, from early childhood education through college, particularly for members of the community served.
Chapter 1 Plan Measures
Priority 2: Increase the number of Wisconsinites with access to quality health care.
Priority 3: Increase and prioritize health improvement approaches that engage, center, and benefit populations and communities at highest risk of health-related inequities.
Chapter 2
Risk Reduction
Chapter 2 Overview

Select a priority to learn more
- Priority 1 Decrease tobacco use and exposure to tobacco.
- Priority 2 Increase physical activity and healthy eating.
- Priority 3 Decrease excessive alcohol consumption.
- Priority 4 Increase cancer prevention vaccine completion.
- Priority 5 Decrease exposure to ultraviolet radiation.
- Priority 6 Decrease exposure to radon.
Many cancer cases in Wisconsin can be prevented.
While some risk factors such as age or genetic risk cannot be changed, other risk factors such as health behaviors can be modified to lower risk and prevent disease.
The World Health Organization estimates that 30 to 50 percent of all cancer cases are preventable.1 In the United States, health behaviors such as smoking and excessive alcohol consumption contribute to 42 percent of all cancer cases and 45.1 percent of all cancer deaths.2
In Wisconsin, we can reduce cancer risk significantly by:
- decreasing tobacco use and exposure.
- decreasing high-risk alcohol consumption.
- maintaining a recommended weight through physical activity and healthy diet.
- increasing protective behaviors from sun and UV exposure.
- increasing HPV and Hepatitis B vaccine utilization.
- reducing exposure to radon.
Personal health behaviors are strongly influenced by the environments in which we live, work, learn, and play. Environments that support health are those that include strong clean air laws; limited alcohol outlet density; access to safe green space, access to healthy food that is affordable and culturally appropriate; access to affordable preventive health care services; radon testing in homes and schools; workplace safety protections, and other structural factors that contribute to the personal health behaviors affecting cancer risk.
The Takeaway
Changes to certain health behaviors can reduce cancer cases and prevent cancer deaths significantly. We can reduce risk and prevent cancer by supporting health behavior changes, and by ensuring that every community has the resources needed to support healthy environments.
Together, we can reduce the risk of developing and dying from cancer.
Key Terms
Alcohol outlet density: The number of places where alcoholic beverages are sold (bars, liquor stores, etc.), either per physical area or per population.3
Binge drinking: A pattern of drinking that brings a person’s blood alcohol concentration (BAC) to 0.08 grams percent or above. This typically happens when men consume 5 or more drinks or women consume 4 or more drinks in about two hours.4
Built environment: All the physical parts of where we live, work, learn, play, and worship (e.g., homes, schools, buildings, streets, open spaces, and infrastructure). The built environment influences a person’s level of physical activity.5
Commercial tobacco: Tobacco that is manufactured by companies for recreational and habitual use in cigarettes, smokeless tobacco, pipe tobacco, cigars, hookahs, and other products. Commercial tobacco is mass-produced and sold for profit. It contains thousands of chemicals and produces over 7,000 chemical compounds when burned, many of which are carcinogenic, cause heart and other diseases, and premature death. This is different from traditional tobacco incorporated into sacred Native American traditions.6
E-cigarette: Battery-powered devices that work by heating a liquid into an aerosol that the user inhales and exhales. These products can be used to deliver nicotine, cannabis (THC and/or CBD), flavorings, chemicals, and other substances. E-cigarettes may be called by different names, such as electronic smoking devices, e-cigs, e-hookahs, vapes, vape pens, tank systems, electronic nicotine delivery systems (ENDS), pod-mods, or mods.7
Food desert: Parts of a community where it is hard to access healthy and affordable food. Food deserts may contribute to disparities in diet and diet-related health outcomes.8
Healthy diet: A diet that emphasizes fruits, vegetables, whole grains, and fat-free or low-fat milk and milk products; includes lean animal-based proteins and/or plant-based proteins; is low in saturated fats, trans fats, cholesterol, salt (sodium), and added sugars; and stays within a person’s daily calorie needs.9
Heavy drinking: For men, heavy drinking means consuming 15 drinks or more per week. For women, heavy drinking means consuming 8 drinks or more per week.4
Hepatitis B: A vaccine-preventable liver infection caused by the hepatitis B virus, which may progress into liver damage and subsequent cancer.10
Human papillomavirus (HPV): A virus with more than 100 types that can infect the genital areas, mouths, and throats of males and females. HPV causes six types of vaccine-preventable cancer: oropharyngeal (back of the throat, including the base of the tongue and tonsils), cervical, vulvar, vaginal, anal, and penile.11
Obesity: Having a weight that is higher than what is recommended for a given height. Obesity results from a combination of causes and contributing factors, including individual factors and environmental factors such as access to healthy food and opportunities for physical activity, education, and exposure to food marketing.12
Radon: A radioactive gas that forms naturally when uranium, thorium, or radium break down in rocks, soil, and groundwater. People can be exposed when they inhale radon-containing air that comes through cracks and gaps in homes, schools, and other buildings. Radon exposure can lead to lung cancer.13
Radon mitigation: Any process or action that is done to reduce radon levels in a building or home.14
Recommended weight: Body Mass Index (BMI), which is based on a person’s height and weight, is an important screening tool for weight categories that are associated with other health problems. If an adult has a BMI within the normal parameters, they are considered to be at a recommended weight.15
SBI (Screening and Brief Intervention) and e-SBI (Electronic Screening and Brief Intervention): The tool providers use to assess patients’ drinking patterns; patients who screen positive for excessive drinking are offered a brief, face-to-face intervention that includes information about the risks of excessive drinking, how to change drinking patterns, and referral to treatment if appropriate. This can also be performed using electronic devices (e.g., computers, telephones, or mobile devices). 16
Standard drink: A standard drink is equal to 14 grams (0.6 ounces) of pure alcohol. 4 Generally, this amount of pure alcohol is found in:
- 12 ounces of beer (5% alcohol content)
- 8 ounces of malt liquor (7% alcohol content)
- 5 ounces of wine (12% alcohol content)
- 5 ounces or a “shot” of 80-proof distilled spirits or liquor (40% alcohol content), e.g., gin, rum, vodka, whiskey
References:
- World Health Organization. Cancer Prevention. https://www.who.int/cancer/prevention/en/. Updated 2020. Accessed February 12, 2020.
- Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the united states. CA Cancer J Clin. 2018;68(1):31-54. doi: 10.3322/caac.21440 [doi].
- Centers for Disease Control and Prevention. (2017). Guide for Measuring Alcohol Outlet Density. Retrieved from: https://www.cdc.gov/alcohol/pdfs/CDC-Guide-for-Measuring-Alcohol-Outlet-Density.pdf
- Centers for Disease Control and Prevention. (2020, January 15). Alcohol and Public Health. Retrieved from Frequently Asked Questions about Alcohol: https://www.cdc.gov/alcohol/faqs.htm
- Centers for Disease Control and Prevention. (2011, June). Impact of the Built Environment on Health. Retrieved from: https://www.cdc.gov/nceh/publications/factsheets/impactofthebuiltenvironmentonhealth.pdf
- Keep It Sacred. (n.d.) Commercial Tobacco. Retrieved from http://keepitsacred.itcmi.org/tobacco-and-tradition/commercial-tobacco/
- Centers for Disease Control and Prevention. (2020, February 24). Smoking & Tobacco Use. Retrieved from About Electronic Cigarettes: https://www.cdc.gov/tobacco/basic_information/e-cigarettes/about-e-cigarettes.html
- Beaulac, J., Kristjansson, E., & Cummins, S. (2009). A Systematic Review of Food Deserts, 1966-2007. Preventing Chronic Disease, 6(3). Retrieved from https://www.cdc.gov/pcd/issues/2009/jul/08_0163.htm
- Centers for Disease Control and Prevention. (2020, March 2). Healthy Eating for a Healthy Weight. Retrieved from Healthy Eating for a Healthy Weight: https://www.cdc.gov/healthyweight/healthy_eating/index.html
- Centers for Disease Control and Prevention. (2020, March 16). Viral Hepatitis. Retrieved from Hepatitis B: https://www.cdc.gov/hepatitis/hbv/index.htm
- Centers for Disease Control and Prevention. (2019, April 29). Human Papillomavirus (HPV). Retrieved from About HPV: https://www.cdc.gov/hpv/parents/about-hpv.html
- Centers for Disease Control and Prevention. (2020, February 4). Overweight and Obesity. Retrieved from Adult Obesity Causes & Consequences: https://www.cdc.gov/obesity/adult/causes.html
- Centers for Disease Control and Prevention. (2020, January 8). National Center for Environmental Health. Retrieved from Protect Yourself and Your Family from Radon: https://www.cdc.gov/features/protect-home-radon/index.html
- Iowa Cancer Consortium. (2018). Iowa Cancer Plan. Retrieved from: https://canceriowa.org/wp-content/uploads/2019/09/2018-2022_Iowa-Cancer-Plan.pdf
- Wisconsin Collaborative for Healthcare Quality and the University of Wisconsin Health Innovation Program. Wisconsin Health Disparities Report, 2019. Retrieved from: https://www.wchq.org/pdfs/Disparities_Report_2019_9-20_FINAL.pdf
- The Community Guide. (2012, August). Alcohol – Excessive Consumption: Electronic Screening and Brief Interventions (e-SBI). Retrieved from https://www.thecommunityguide.org/findings/alcohol-excessive-consumption-electronic-screening-and-brief-interventions-e-sbi
Priority 1: Decrease tobacco use and exposure to tobacco.
Strategy A: Prevent youth access and initiation of tobacco products.
Action Steps
- Increase the percentage of middle and high school youth receiving instructions about why they should not use tobacco products.
- Increase the percentage of middle and high school youth participating in any organized activities to keep people their age from using any form of tobacco product.
- Promote free trainings for retailers regarding Wisconsin tobacco sales law to increase compliance with youth tobacco access laws.
- Educate the general public (parents, teachers, students, local leaders) on the dangers of cigarettes, other commercial tobacco products, and e-cigarettes.
- Increase the cigarette tax.
- Support policies that tax all tobacco products at the same rate.
- Increase policies to restrict youth access and use of cigarettes, other commercial tobacco products, and e-cigarettes.
- Fully fund a Wisconsin comprehensive tobacco prevention and control program consistent with CDC funding recommendations.
- Train community health workers on culturally appropriate strategies to prevent the use of tobacco, e-cigarettes, and other nicotine products.
Strategy B: Protect and strengthen clean air laws.
Action Steps
- Maintain and expand clean air laws and policies to include e-cigarettes.
- Expand clean air laws to include outdoor spaces.
- Increase the availability of smoke-free rental properties.
- Maintain smoke-free multi-unit public housing policy.
Strategy C: Increase access to and use of evidence-based tobacco addiction treatment.
Action Steps
- Promote and support evidence-based cessation resources, especially among populations disparately impacted by commercial tobacco use and e-cigarette use/vaping.
- Encourage health care provider support for evidence-based cessation treatment and resources for patients, especially among behavioral health and substance abuse treatment providers.
- Increase the number of Wisconsin health care systems with capacity to refer patients to the Wisconsin Tobacco Quit Line and the First Breath Program via their electronic health record.
- Support and protect comprehensive, evidence-based cessation insurance benefits among private and public plans.
- Educate community members about available smoking cessation benefits through private and public insurance plans.
- Support and promote the Wisconsin Tobacco Quit Line as a free smoking cessation resource, especially among disparate populations.
- Establish a plan to provide equitable access to evidenced-based tobacco addiction treatment during public health emergencies.
- Train community health workers on culturally appropriate tobacco cessation and employ community health workers to increase access to evidence-based nicotine addiction treatment
Priority 2: Increase physical activity and healthy eating.
Strategy A: Create environments that support physical activity.
Action Steps
- Educate decision-makers on evidence-based policies that create built environments to encourage safe physical activity.
- Identify, examine, and disseminate initiatives throughout the state that address physical activity and chronic disease control with an emphasis on cancer reduction and control.
- Educate decision-makers on evidence-based policies and programs that encourage physical activity within schools and worksites.
- Engage a variety of community partners to address local barriers to physical activity.
- Encourage family and broader social network participation in physical activity.
- Improve access to and utilization of programs and resources that encourage physical activity.
- Support educational campaigns that emphasize the benefits of physical activity and the risks of inactivity.
- Educate decision-makers on evidence-based policies and programs that emphasize the importance of appropriate physical activity during and after cancer treatment.
- Educate decision-makers on evidence-based policies and initiatives to reduce screen time in schools, daycare centers, and after-school programs.
- Incorporate physical activity during screen time, such as virtual physical activity courses.
Strategy B: Create environments that support healthy eating.
Action Steps
- Identify, examine, and disseminate initiatives throughout the state that address nutrition and chronic disease control such as cancer.
- Educate decision-makers on evidence-based policies that increase the availability and affordability of healthy foods and beverages in communities, workplaces, childcare, and school settings, particularly in rural and underserved communities.
- Provide incentives to establish supermarkets, gardens, and farmers’ markets in underserved areas.
- Encourage family and broader social network participation in nutrition.
- Engage a variety of community partners to address local barriers to healthy eating.
- Support educational campaigns that emphasize the importance of healthy eating and healthy cooking in schools, communities, workplaces, and at home.
- Educate decision-makers on evidence-based policies and programs that increase breastfeeding initiation, duration, and exclusivity.
- Educate decision-makers on evidence-based policies and programs that emphasize the importance of healthy eating during and after cancer treatment.
- Incorporate food deserts into community health assessments.
Strategy C: Increase screening for obesity and access to weight management interventions.
Action Steps
- Increase health provider awareness on the importance of nutrition and physical health on various health outcomes with continuing education.
- Develop evidence-based policies and procedures for obesity screening and intervention in primary care.
- Train health care providers on how to identify and treat obesity in their patients.
- Take a health care team-based approach to obesity management.
- Educate parents about the importance of engaging their health care providers in discussions about their child’s weight.
- Promote the use of multicomponent interventions that use technology-supported coaching or counseling to help clients lose or maintain weight.
- Increase insurance coverage and reimbursement for weight management services, such as nutritional and fitness support services.
- Increase nutritional and physical activity services available for cancer survivors and their survivorship needs.
Strategy D: Increase awareness of the connection between obesity, lack of physical activity, and lack of healthy eating and cancer risk.
Action Steps
- Expand and utilize educational materials that define obesity, lack of physical activity, and poor nutrition and its link to cancer.
- Support the development of media campaigns to increase public awareness of the link between obesity, lack of physical activity and poor nutrition and cancer.
- Promote health care provider education and training on obesity, lack of physical activity, and poor nutrition as a risk factor for cancer.
- Employ community health workers to support culturally appropriate strategies to emphasize the importance of healthy eating and physical activity as tools to help prevent cancer
Priority 3: Decrease excessive alcohol consumption.
Strategy A: Increase awareness of the connection between alcohol consumption and cancer risk.
Action Steps
- Expand and utilize educational materials that define excessive alcohol consumption and its link to cancer.
- Support the development of media campaigns to increase public awareness of the link between alcohol use and cancer.
- Promote health care provider education and training on alcohol use as a risk factor for cancer.
- Increase the number of communities addressing high-risk alcohol use that also incorporate the link between alcohol and cancer in their messaging and activities.
- Encourage collaboration with other chronic disease programs to promote awareness of alcohol use as a risk factor for cancer.
Strategy B: Create community environments that prevent and reduce the excessive use of alcohol.
Action Steps
- Increase the alcohol tax.
- Increase local policies that limit the availability of alcohol in public spaces.
- Increase local policies that discourage excessive alcohol consumption.
- Support efforts to prevent underage drinking, including the maintenance and enforcement of Wisconsin social host laws; enhanced enforcement of laws prohibiting sales to those underage; local efforts to reduce youth exposure to alcohol advertising; and alcohol education starting at age 8 and continuing in all remaining levels of education.
- Support workplace policies to prevent and reduce excessive drinking.
- Limit the number and location of alcohol outlets by population size.
- Encourage and support alcohol-free and recovery friendly public environments, events, parks, and venues.
- Establish a state level measure to track policies introduced and passed aimed to reduce excessive alcohol consumption.
Strategy C: Increase screening and treatment for excessive alcohol use.
Action Steps
- Train health care providers on how to screen and provide brief interventions to patients for excessive alcohol consumption.
- Promote existing community resources that address excessive alcohol consumption.
- Maintain reimbursement for the screening and treatment of excessive alcohol use.
- Educate community members and providers about the availability of addiction treatment insurance benefits.
- Use culturally and linguistically competent tools to prevent and reduce excessive drinking.
- Promote the use of electronic screening and brief intervention (e-SBI) to facilitate the delivery of personalized feedback about the risks and consequences of excessive drinking.
Priority 4: Increase cancer prevention vaccine completion.
Strategy A: Increase access to cancer prevention vaccination services.
Action Steps
- Increase the availability of extended clinic hours for vaccination opportunities.
- Allow non-physician health care providers to vaccinate all eligible patients, provided they are appropriately trained and educated.
- Encourage the use of standing orders in health systems to allow non-physicians to administer vaccines.
- Promote vaccination in schools.
- Utilize school-based clinics to vaccinate children.
- Establish cancer prevention vaccination requirements for school enrollment.
- Require all insurance carriers to cover the complete cancer prevention vaccine series for all eligible patients at no cost.
- Maintain funding for Vaccines for Children program to provide no-cost vaccinations to Medicaid eligible, underinsured, uninsured, and American Indian/Alaskan Native children.
- Increase funding for local health departments to administer cancer prevention vaccines.
- Include vaccination programs in the Special and Supplemental Nutrition Program for Women, Infants, and Children (WIC).
- Implement client or family incentive rewards for vaccination programs.
- Establish a plan to provide equitable access to cancer prevention vaccines during public health emergencies.
- Employ community health workers to increase cancer prevention vaccine completion.
Strategy B: Increase provider, parent, caregiver, and patient acceptance of cancer prevention vaccines.
Action Steps
- Create media campaigns to inform the public on the value of the HPV and Hepatitis B vaccines as cancer prevention.
- Develop tailored, culturally appropriate, and accessible educational campaigns, especially for patients with low vaccination rates and their caregivers.
- Work with local immunization coalitions to disseminate information about cancer prevention vaccines to their communities.
- Educate policymakers on the purpose of cancer prevention vaccines.
- Educate policymakers on the underutilization of cancer prevention vaccines.
- Educate policymakers about the safety of cancer prevention vaccines and importance in cancer prevention.
- Reduce vaccine opt-out exemptions.
- Share immunization rates regularly with the public.
- Encourage the use of diverse personal stories and community voices to reduce stigma around cancer prevention vaccines.
- Engage faith-based communities in education and messaging opportunities about cancer prevention vaccines.
- Educate parents, medical providers, and policymakers on the increasing incidence of oropharyngeal cancer and HPV vaccination as a solution for rising cancer rates.
Strategy C: Reduce missed clinical opportunities to recommend and administer cancer prevention vaccines.
Action Steps
- Encourage and train doctors, nurses, and other health care professionals to provide strong recommendations on the benefits of vaccinations preventing cancer.
- Encourage birthing hospitals and centers to complete universal hepatitis B vaccination within 24 hours of birth, followed by completion of the vaccine series per Advisory Committee on Immunization Practices (ACIP) recommendations.
- Administer hepatitis B vaccine and hepatitis B immune globulin (HBIG) for infants born to hepatitis B surface antigen positive women within 12 hours of birth to prevent infection.
- Train health care providers to review patient vaccine history at all medical encounters and administer cancer prevention vaccines due at all medical encounters.
- Implement different methods (phone, text, email) to remind patients and caregivers to receive cancer prevention vaccines and follow-up doses.
- Offer cancer prevention vaccine continuing medical education for primary care, family medicine, obstetrics, and advanced practice health care providers.
- Maintain and promote the statewide publicly reported metric on the achievement of cancer prevention vaccine completion.
- Identify adult patients with incomplete cancer prevention vaccine series but still within the recommended age group and encourage them to complete the vaccine series.
- Identify and address disparities related to vaccine uptake and completion.
- Create tailored interventions that reduce missed opportunities in populations with the lowest vaccine uptake.
- Educate the public and providers on vaccine guideline changes such as universal hepatitis B vaccination for adults ages 18-59 and permissive guidance age 60+.
Priority 5: Decrease exposure to ultraviolet radiation.
Strategy A: Increase opportunities for sun protection in outdoor settings.
Action Steps
- Increase availability and use of shade structures in outdoor settings, including schools, worksites, and recreational sites.
- Increase availability and use of SPF 15 or higher sunscreen in outdoor settings, including schools, worksites, and recreational sites.
- Educate decision-makers on evidence-based policies that increase availability and use of shade structures and SPF 15 or higher sunscreen in both public and private outdoor spaces.
- Increase availability and use of shade structures and sunscreen in low-income communities.
Strategy B: Increase awareness about skin cancer prevention.
Action Steps
- Train education professionals to reinforce skin protective behaviors for youth by modeling, demonstration, and role-playing.
- Encourage health care providers to educate patients about skin protective behaviors.
- Increase targeted skin cancer education for outdoor workers.
- Tailor education and awareness activities for populations with darker complexions to normalize skin protective behaviors.
- Track and monitor the number of policies introduced and passed to reduce skin cancer.
Strategy C: Decrease indoor tanning use.
Action Steps
- Educate policymakers on evidence-based policies that reduce indoor tanning use, especially among youth.
- Maintain and follow Federal Drug Administration regulations on indoor tanning use.
- Reduce youth access to indoor tanning.
- Develop and implement a public awareness campaign to highlight the dangers of indoor tanning.
- Decrease availability of indoor tanning in health and wellness facilities, such as fitness centers and spas.
Priority 6: Decrease exposure to radon.
Strategy A: Increase awareness of the connection between radon and cancer risk.
Action Steps
- Educate the public, health care providers, public health officials, schools, property owners, property managers, and policymakers about radon and other environmental substances linked to cancer.
- Create and tailor educational and awareness materials on the link between radon and cancer risk.
- Promote educational materials in health care facilities, schools, and at home shows.
- Integrate educational materials into real estate and rental documents.
- Establish requirements to inform homeowners and tenants of radon and its risk for lung cancer.
- Track and monitor the number of policies introduced and passed to reduce radon exposure.
Strategy B: Increase the testing for and mitigation of radon in homes and other buildings.
Action Steps
- Increase the percentage of Wisconsinites who test their homes for radon and mitigate when needed.
- Increase accessibility and availability of radon testing and mitigation services.
- Collaborate with cities and housing departments to develop initiatives that provide financial assistance for radon testing and mitigation.
- Tailor outreach and awareness efforts for radon testing and mitigation services.
- Develop data collection standards to monitor testing and mitigation of homes and buildings in Wisconsin.
- Require radon testing and mitigation in schools, multi-unit housing, rental housing, and new construction projects.
- Require radon tests be performed prior to the sale of single-family homes.
- Establish a plan to provide equitable access to radon testing and mitigation services during public health emergencies.
Strategy C: Increase the number of residential buildings built or remodeled using radon reducing methods.
Action Steps
- Develop an awareness campaign about radon-resistant construction techniques and methods.
- Develop data collection standards to monitor radon-resistant construction.
- Support building codes that require newly constructed homes and buildings to use passive radon control methods.
- Increase qualified radon mitigation professionals in Wisconsin.
Chapter 2 Plan Measures
Priority 1: Decrease tobacco use and exposure to tobacco.
Priority 2: Increase physical activity and healthy eating.
Priority 3: Decrease excessive alcohol consumption.
Priority 4: Increase cancer prevention vaccine completion.
Priority 5: Decrease exposure to ultraviolet radiation.
Priority 6: Decrease exposure to radon.
Chapter 3
Early Detection and Screening
Chapter 3 Overview

Select a priority to learn more
- Priority 1 Increase awareness and demand for recommended cancer screenings.
- Priority 2 Implement health care systems-level strategies to increase recommended cancer screenings and diagnostic services.
- Priority 3 Increase access to recommended cancer screenings.
- Priority 4 Increase utilization of cancer genetic risk assessment and counseling.
Screening for cancer can save lives.
Screening and early detection can find cancer at earlier stages when it is easier to treat, and can identify pre-cancers that can be addressed before cancer occurs.
Some patients and families have a higher genetic risk for certain cancers. Genetic counseling and testing can help identify patients who may need increased cancer screening or screening at earlier ages.
Cancer screening recommendations can evolve and develop over time. As of 2020, the US Preventive Services Task Force (USPSTF) recommends screening guidelines for breast, cervical, colorectal, and lung cancers based on current evidence. The Affordable Care Act of 2010 requires that insurers cover these cancer screenings and other preventative services recommended by the USPSTF. Health care providers and patients should determine which cancer screenings are needed based on a patient’s individual risk.
The routine use of cancer screenings can dramatically reduce mortality. However, significant disparities must be addressed to ensure equitable cancer screening benefits for all Wisconsinites.
Cancer screening efforts in Wisconsin
As of 2018, Wisconsin screening rates for breast, cervical, and colorectal cancers were around or above national averages1:
- 67 percent of women ages 45 years and older had an up-to-date mammography.
- 88 percent of women ages 21-65 had received a Pap and/or HPV test.
- 74 percent of women and men ages 50 and older had received a stool test and/or endoscopy (including either flexible sigmoidoscopy or colonoscopy).
Unfortunately, specific populations in Wisconsin experience significant disparities in screening access and completion. For example, while overall colorectal cancer screening in Wisconsin is on the rise, rates are much lower among African Americans than among whites. Screening occurred more frequently in women and people aged 65 to 75, who were likely insured by Medicare.2
Screening disparities can lead to considerable differences in mortality rates and often are caused by barriers such as:
- limited clinic hours
- transportation access
- the perceived (or actual) cost of screening, diagnostic, and follow-up care
- access to diagnostic and follow-up care
- inadequate provider communication or follow-up
- biased care
- fear of stigma
- fear of the financial, emotional, and/or other impacts of a cancer diagnosis
- lack of accessible information regarding why screening is important
The Takeaway
Timely recommended screenings can prevent disease and suffering. We can reduce barriers to ensure all Wisconsinites are able to access and complete the cancer screenings they need.
Together, we can save lives and reduce suffering by detecting cancer at the earliest stage possible.
Key Terms
Genetic counseling: A communication process between a specially trained health professional and a person concerned about their genetic risk of disease. The person’s family and personal medical history may be discussed, and counseling may lead to genetic testing.3
Genetic risk: The increased likelihood of developing a disease based on a person’s genetic makeup. This may include family history, genetic variations and/or mutations, and behavioral or environmental factors that interacts with genetics.4
Genetic testing: The process of analyzing a patient’s sample (usually blood or saliva) for changes in the inherited material (DNA which is made up of genes) to determine if there is a predisposition to developing a health condition, such as cancer. Another type of genetic testing is called molecular profiling (using tumor tissue or circulating tumor DNA in the blood) which looks for acquired changes in the tumor DNA to help diagnose cancer, determine treatment, or find out how well treatment is working.5
Structural barriers: Non-economic obstacles that make it difficult for people to access cancer screening. These could include barriers such as transportation, hours and locations of services, referral processes, translation services, among other factors.6
References:
- American Cancer Society. (2020). Wisconsin At a Glance. Retrieved from: https://cancerstatisticscenter.cancer.org/#!/state/Wisconsin
- Centers for Disease Control and Prevention. (2016). Colorectal Cancer (CRC) Screening in Wisconsin. Retrieved from https://www.cdc.gov/cancer/ncccp/screening-rates/pdf/colorectal-cancer-screening-wisconsin-508.pdf
- National Cancer Institute. (2020, February 28). Cancer Genetics Risk Assessment and Counseling (PDQ®)–Health Professional Version. Retrieved from Genetic Counseling: https://www.cancer.gov/about-cancer/causes-prevention/genetics/risk-assessment-pdq
- National Cancer Institute. (2020, February 28). Genetics. Retrieved from Cancer Genetics Risk Assessment and Counseling (PDQ®)–Health Professional Version: https://www.cancer.gov/about-cancer/causes-prevention/genetics/risk-assessment-pdq
- National Cancer Institute. (2019, March 15). Genetics. Retrieved from Genetic Testing for Inherited Cancer Susceptibility Syndromes: https://www.cancer.gov/about-cancer/causes-prevention/genetics/genetic-testing-fact-sheet
- The Community Guide. (2013, September 25). Community Preventative Services Task Force. Retrieved from: https://www.thecommunityguide.org/sites/default/files/assets/Cancer-Screening-Reducing-Structural-Barriers.pdf
Priority 1: Increase awareness and demand for recommended cancer screenings.
Strategy A: Develop public awareness campaigns designed to reach communities and populations at greatest need for cancer screening.
Action Steps
- Develop and implement public awareness campaigns to educate the public on the importance of cancer screenings.
- Create awareness campaigns at schools, worksites, and communities to inform the public on current screening recommendations and options.
- Develop culturally and linguistically appropriate information on cancer screening recommendations.
- Educate communities about risk factors, including family history, which may change standard cancer screening recommendations.
- Educate community members about the health benefits of available cancer screenings through private and public insurance plans.
- Encourage Insurers to promote screening activities with their consumers.
Strategy B: Increase the availability of community-driven and peer-to-peer education to increase utilization of recommended cancer screenings.
Action Steps
- Inform the public on current screening recommendations through schools, worksites, and communities.
- Develop culturally and linguistically appropriate and community-driven information on cancer screening recommendations.
- Implement peer-to-peer education and community health worker models to increase the utilization of recommended cancer screenings.
- Educate community members about available cancer screening benefits through private and public insurance plans.
- Educate communities, including faith-based communities, on the importance of sharing and obtaining a family cancer history.
- Assess and share best practice models on community education to increase recommended cancer screening utilization.
- Support existing outreach efforts and community-based projects to increase the recommended cancer screening utilization.
Priority 2: Implement health care systems-level strategies to increase recommended cancer screenings and diagnostic services.
Strategy A: Encourage health systems to identify or develop quality improvement metrics and processes to improve cancer screening rates and diagnostic services.
Action Steps
- Establish a statewide quality improvement measure for lung cancer screening.
- Gather data and conduct assessments to identify specific populations with low rates of recommended cancer screening utilization.
- Create a quality improvement team and plan to increase rates among patient population groups with the lowest screening rates.
- Reduce time between initial screening and diagnostic services for individuals whose results may indicate cancer, when necessary.
- Track and share quality improvement results.
- Foster an environment of continuous quality improvement to promote an organizational culture of clinical care improvement.
- Utilize tested quality improvement strategies (Plan-Do-Study-Act (PDSA) cycles, process mapping, root-cause analysis, etc.).
- Provide low-cost or free cancer screening opportunities to increase demand and participation.
- Celebrate successes when goals or objectives are achieved to maintain excitement around quality improvement activities.
Strategy B: Create opportunities and tools for providers and patients to remain up-to-date on current cancer screening recommendations.
Action Steps
- Implement provider reminder systems that identify patients due for recommended cancer screenings.
- Utilize patient reminder tools to inform patients that they are due for cancer screenings.
- Implement shared decision-making tools to incorporate family history, previous screening experience, and/or behavioral risks into screening recommendations.
- Establish a cancer screening registry to track when cancer screenings are due.
- Offer continuing education and training opportunities for health care providers on current cancer screening recommendations and communication best practices.
- Provide simple language and tools for health care providers to use to discuss screening recommendations with patients.
- Increase the availability of culturally and linguistically appropriate patient navigation systems within health systems to increase the utilization of recommended screenings.
- Recognize clinics and providers that routinely recommend and/or screen patients for cancer.
Priority 3: Increase access to recommended cancer screenings.
Strategy A: Reduce structural barriers to cancer screening.
Action Steps
- Define common screening barriers, particularly those unique to underserved communities.
- Promote full insurance coverage for recommended cancer screenings, including diagnostic screenings.
- Keep decision-makers informed on the current recommendations for cancer screenings.
- Increase the availability of extended clinic hours to offer screening services.
- Promote and support programs that provide free or low-cost recommended screenings to the under and uninsured.
- Participate in or establish free and low-cost screening programs for patients.
- Provide information to health care providers and patients about the availability of free and low-cost screenings and how to access them.
- Create tax incentives for facilities that offer recommended cancer screenings for free or at a reduced rate.
- Increase access to recommended screenings among rural and isolated populations.
- Provide screening services in non-traditional clinic settings.
- Provide transportation for screening services or reimbursement for travel costs.
- Provide paid time off work for employees to utilize screening services.
- Monitor policies introduced and passed regarding cancer screening, including attempts to address loopholes in coverage and costs associated with diagnostics and follow-up.
- Reduce barriers to timely diagnostic and follow-up care.
- Establish a plan to provide equitable access to cancer screening during public health emergencies.
Strategy B: Increase insurance coverage for diagnostic testing.
Action Steps
- Provide full insurance coverage for diagnostic testing, including after a positive or inconclusive screening result.
- Encourage insurers to promote screening activities with their consumers.
- Educate policymakers on the importance of diagnostic and follow-up care.
- Establish insurance coverage for patient navigators and navigation services provided.
- Utilize financial navigators to help patients navigate paying for diagnostic services.
- Train patient navigators on culturally and scientifically appropriate language to explain diagnostic and follow-up care.
- Maintain patient protections for pre-existing conditions.
- Inform patients and their care teams of legal insurance coverage requirements.
- Monitor policies introduced and passed regarding cancer screening and diagnostic testing.
- Ensure any medically necessary follow-up testing after an abnormal screening test is covered as part of the initial screening.
Strategy C: Increase community-clinical linkages to recommended cancer screening services.
Action Steps
- Increase health care system work with community- and faith-based organizations to improve the availability of culturally and linguistically appropriate patient navigation systems within communities to increase utilization of recommended screenings.
- Employ community health workers to increase cancer screening.
- Empower faith-based communities to educate members on cancer screening recommendations.
- Inform community members about available cancer screening benefits through private and public insurance plans.
- Provide community opportunities to access low-cost or free early detection cancer screenings.
- Promote mobile screening services to increase access and availability.
Priority 4: Increase utilization of cancer genetic risk assessment and counseling.
Strategy A: Educate providers and patients about assessing genetic cancer risk.
Action Steps
- Train the health care team on the importance of cancer genetic risk assessment and counseling.
- Create a targeted public awareness campaign on what cancer genetic risk assessment and counseling are and their importance.
- Provide culturally and linguistically appropriate cancer genetic risk assessment materials to providers and patients.
Strategy B: Increase the availability of cancer genetic risk assessments and counseling.
Action Steps
- Develop provider reminder systems for cancer genetic risk assessment and counseling.
- Train health professionals to conduct initial cancer risk assessments and refer patients to a qualified cancer genetic counselor when appropriate.
- Partner with professionals other than genetic counselors, such as nurse educators, to provide cancer risk assessments and counseling.
- Promote the benefits of having qualified cancer genetic counselors on staff to health care systems.
- Integrate genetic counseling into the patient care teams at oncology clinics.
- Utilize secure telehealth technology and services to increase access to genetic counseling.
- Educate policymakers on the role of state licensure in ensuring a qualified cancer genetic counselor workforce.
- Promote the development of more graduate programs in Wisconsin to train qualified cancer genetic counselors.
- Establish a plan to provide equitable access to cancer genetic risk assessment and counseling during public health emergencies.
Strategy C: Establish insurance coverage for cancer genetic risk assessment and counseling.
Action Steps
- Assess gaps in health insurance coverage and identify policy opportunities to address those gaps.
- Educate policymakers on the benefits of cancer genetic risk assessments and counseling.
- Educate insurance companies about the benefits and cost-saving potential of cancer genetic risk assessments and counseling.
- Expand cancer genetic risk assessment and counseling services covered by Medicare and Medicaid.
- Establish and expand coverage for secure telehealth technology and services to increase access to genetic counseling.
Chapter 3 Plan Measures
Priority 1: Increase awareness and demand for recommended cancer screenings.
Priority 2: Implement health care systems-level strategies to increase recommended cancer screenings and diagnostic services.
Priority 3: Increase access to recommended cancer screenings.
Priority 4: Increase utilization of cancer genetic risk assessment and counseling.
Chapter 4
Treatment
Chapter 4 Overview
Select a priority to learn more
- Priority 1 Increase availability and access to quality cancer care.
- Priority 2 Increase availability and access to palliative care early and throughout treatment.
- Priority 3 Increase patient and caregiver access to non-clinical support services, including care coordination, patient navigation, psychosocial support, and rehabilitation services.
- Priority 4 Increase participation in clinical trials.
- Priority 5 Increase the number of advance care planning conversations for all cancer patients early in their treatment.
An estimated 35,280 new cancers will be diagnosed among Wisconsinites in 2020.1
The majority of these patients will seek active treatment with the goal of curing the disease and/or prolonging life.
While cancer remains a leading cause of death in Wisconsin, advances in treatment are responsible, in part, for the state’s growing population of cancer survivors. Put simply, quality and timely cancer treatment can save lives.
Unfortunately, Wisconsinites can face numerous barriers in accessing cancer treatment that is quality, timely, and affordable. These barriers can include but are not limited to: delayed diagnosis, insurance coverage, distance from cancer treatment facilities, and difficulty navigating the complex health care system.
Cancer treatments can take a physical, mental, emotional, social, and financial toll on patients, their caregivers, and support systems. In addition, the cost of treatment can create significant and lasting hardship for survivors and families. In numerous national studies, 48 to 73 percent of cancer survivors reported adverse financial effects resulting from the high costs of cancer treatments.2, 3
Fortunately, credible, evidence-based treatment guidelines can be used to reduce variation in the provision of cancer care, thereby improving health outcomes, patient well-being, and the cost-effectiveness of care.
What are common treatment options*?
- Surgery: a procedure in which a surgeon removes cancer from the body
- Radiation therapy: a type of cancer treatment that uses high doses of radiation to kill cancer cells and shrink tumors
- Chemotherapy: a type of cancer treatment that uses drugs to kill rapidly growing cells, including cancer cells
- Immunotherapy: a type of cancer treatment that helps boost the body’s own immune system to treat cancer
- Targeted therapy: a type of cancer treatment that uses unique parts of the cancer cells to kill cancer cells and tumors
- Hormone therapy: a treatment that slows or stops the growth of breast and prostate cancers that use hormones to grow
- Palliative care: care given in conjunction with other treatment or by itself to maximize the quality of life and comfort of patients who have a serious or life-threatening disease
*People with cancer may have only one treatment or various combinations of treatments, depending on the type, stages, and location of the cancer. There may be other treatments not listed here.
Key Terms
Advance care planning: The process of deciding and sharing a person’s preferences about receiving health care if they later become unable to speak for themselves. These preferences are usually stated in documents called advance directives.4
Advance directives: Legal documents that states a person’s wishes about receiving medical care if that person is no longer able to make medical decisions because of a serious illness or injury. Advance directives also may give a person the authority to make medical decisions for another person when that person can no longer make decisions for themselves.5 These documents generally include a health care power of attorney and a living will.
Caregiver: A person who gives care to someone living with a cancer diagnosis. Caregivers may be family members, friends, health professionals, social workers, or members of the clergy. They may give care at home or in a hospital or other health care setting.6
Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. Chemotherapy may be given by mouth, injection (intravenous or otherwise), infusion, or on the skin, depending on the type and stage of the cancer being treated. It may be given alone or with other treatments, such as surgery, radiation therapy, or immunotherapy.7
Clinical trials: A type of research study that tests how well new medical approaches work in people. Clinical trials are used to test new methods of screening, prevention, diagnosis, or treatment of a disease. Also called clinical study.8
Genetic testing: The process of analyzing a patient’s sample (usually blood or saliva) for changes in the inherited material (DNA which is made up of genes) to determine if there is a predisposition to developing a health condition, such as cancer. Another type of genetic testing is called molecular profiling (using tumor tissue or circulating tumor DNA in the blood) which looks for acquired changes in the tumor DNA to help diagnose cancer, determine treatment, or find out how well treatment is working.9
Immunotherapy: A type of treatment that uses substances to stimulate the immune system to help the body fight cancer, infection, and other diseases.10
Palliative care: Care given to improve the quality of life of patients who have a serious or life-threatening disease. The goal of palliative care is to prevent or reduce the symptoms of a disease, side effects caused by treatment, and the psychological, social, and spiritual problems related to a disease or its treatment. Also called palliative medicine, comfort care, supportive care, and symptom management. Palliative care can begin at any time during treatment and can occur alongside curative treatment when resources are available.11
Prior authorization: A decision by a health insurer that a particular health care service, treatment plan, prescription drug, or medical equipment is medically necessary. Sometimes called prior approval or precertification.12
Quality of life: The overall enjoyment of life, including an individual’s sense of well-being and ability to carry out various everyday activities.13
Support services: Non-medical support, information, and financial resources available to cancer patients and caregivers.14
The Takeaway
Every Wisconsinite deserves access to affordable, timely, quality cancer treatment options. New cancer treatments and research are emerging, offering hope and promise. Further work is necessary to eliminate barriers to treatment and reduce both the financial repercussions and the health side effects that negatively affect cancer survivors and their support systems.
Together, we can increase access to quality cancer care, non-clinical supports, and clinical trials, to reduce death and suffering caused by cancer.
What populations are underrepresented in cancer-related clinical trials?
- All racial and ethnic minority groups
- Persons living in rural areas
- Persons with longer travel distances to receive trial services
- Persons living with low socioeconomic status
- Persons who speak English as their second language
- Persons living with medically complex situations (such as persons living with HIV)
- Older adults
- Populations that require additional research oversight
References:
- American Cancer Society. (2020). Wisconsin At a Glance. Retrieved from: https://cancerstatisticscenter.cancer.org/#!/state/Wisconsin
- Gordon, L. G., Merollini, K. M., Lowe, A., & Chan, R. J. (2017). A systematic review of financial toxicity among cancer survivors: we can’t pay the co-pay. The Patient-Patient-Centered Outcomes Research, 10(3), 295-309.
- Lentz, R., Benson III, A. B., & Kircher, S. (2019). Financial toxicity in cancer care: Prevalence, causes, consequences, and reduction strategies. Journal of surgical oncology, 120(1), 85-92.
- National Institutes of Health. (2018, January 15). National Institute on Aging. Retrieved from Advance Care Planning: Healthcare Directives: https://www.nia.nih.gov/health/advance-care-planning-healthcare-directives
- National Cancer Institute. (2015, March 10). Advance Directives. Retrieved from https://www.cancer.gov/about-cancer/managing-care/advance-directives
- National Cancer Institute. (2020, January 3). Coping with Cancer. Retrieved from Support for Caregivers of Cancer Patients: https://www.cancer.gov/about-cancer/coping/caregiver-support
- National Cancer Institute. (2015, April 29). Chemotherapy to Treat Cancer. Retrieved from https://www.cancer.gov/about-cancer/treatment/types/chemotherapy
- National Cancer Institute. (2020, February 4). Clinical Trials Information. Retrieved from What Are Clinical Trials: https://www.cancer.gov/about-cancer/treatment/clinical-trials/what-are-trials
- National Cancer Institute. (2019, March 15). Genetics. Retrieved from Genetic Testing for Inherited Cancer Susceptibility Syndromes: https://www.cancer.gov/about-cancer/causes-prevention/genetics/genetic-testing-fact-sheet
- National Cancer Institute. (2019, September 24). Types of Cancer Treatment. Retrieved from Immunotherapy to Treat Cancer: https://www.cancer.gov/about-cancer/treatment/types/immunotherapy
- National Cancer Institute. (2017, October 20). Palliative Care in Cancer. Retrieved from https://www.cancer.gov/about-cancer/advanced-cancer/care-choices/palliative-care-fact-sheet
- gov. (n.d.). Preauthorization. Retrieved from https://www.healthcare.gov/glossary/preauthorization/
- National Cancer Institute. (n.d.). NCI Dictionary of Cancer Terms. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms
- National Cancer Institute. (2019, November 8). Support Services. Retrieved from https://www.cancer.gov/about-cancer/managing-care/services/support
Priority 1: Increase availability and access to quality cancer care.
Strategy A: Reduce time between diagnosis and treatment.
Action Steps
- Reduce barriers for health care providers, such as insurance prior authorization requirements, for recommending treatments, imaging genetic and molecular lab testing, and other lab/radiology procedures.
- Improve coordination of care between health facilities and systems throughout diagnosis and post-treatment.
- Create and implement quality improvement projects to reduce the time between diagnosis and treatment.
- Recruit and train patient navigators and community health workers to help guide the next steps for patients and caregivers.
- Recruit and train diverse patient navigators and community health workers that are representative of the communities they are serving.
- Engage patient navigators to educate patients and caregivers on the importance of timely informed decision-making, including potential long-term and late effects of care.
- Encourage health systems and institutions to adopt available cancer information resources and referral systems.
- Promote full insurance coverage for recommended cancer screenings, and diagnostic tests following inconclusive or positive screening results.
Strategy B: Increase conversations between patients, families, and providers about treatment options and goals of care.
Action Steps
- Develop patient and caregiver education resources to address shared decision-making.
- Develop and disseminate tools for shared decision-making to patients and their families.
- Train health care providers on how to have conversations that include the patient in setting goals of care.
- Provide multiple opportunities for patients to discuss, establish, and maintain goals of care with their care team as their treatment progresses.
- Train providers on how to foster multiple opportunities for patients to discuss their goals of care with their providers as treatment progresses.
- Increase the length of appointments to allow for increase conversations between patients and providers.
- Develop and disseminate culturally and linguistically appropriate materials for supporting conversations about goals of care.
- Employ patient navigators and community health workers to support and teach patients to be a partner in setting goals of care.
- Increase insurance coverage and reimbursement for sexual health and fertility planning services and discussions before, during, and after treatment for certain cancers.
- Include long-term risks of treatment (including second cancers) in discussions before, during, and after treatment for certain cancers.
- Educate patients early in their treatment about palliative care and its role in their treatment.
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients.
- Encourage health systems and institutions to adopt available cancer information resources and referral systems.
- Discuss other ways for patients to participate in research, in addition to clinical trials.
Strategy C: Increase use of treatment guidelines and quality care standards.
Action Steps
- Create electronic health record algorithms for the delivery of standards of care.
- Develop provider incentives for compliance with the American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN) standards.
- Develop statewide publicly reported metrics for provider adherence to standards of care.
- Educate health care providers on evidence-based, best practices in cancer care.
- Increase cancer care facilities with Commission on Cancer accreditation.
- Encourage health systems to have supportive care team members on staff to minimize referrals needed, such as patient navigators, social workers, genetic risk counselors, nutritionists, psychiatrists, and rehabilitation therapists.
- Educate health care professionals on recommendations/standards for follow-up care for pediatric cancer survivors (e.g., Children’s Oncology Group/COG Guidelines) that should be followed.
- Cancer treatment facilities develop a plan which can be rapidly implemented to address chemotherapy shortages as they occur.
Strategy D: Increase community-clinical linkages to reduce structural barriers to accessing cancer treatment.
Action Steps
- Support the implementation of evidence-based policy and systems change to reduce transportation-related barriers in receiving recommended cancer treatments.
- Utilize secure telehealth technology and services to increase access to care.
- Create and provide resources and information for all patient languages, including translators, interpreters, and the use of translation technology when needed.
- Create and maintain high-quality community engagement programs to establish relationships between community members and cancer treatment facilities.
- Recruit, train, and employ community members to be patient navigators in the community in which they reside.
- Recruit, train, and employ patient navigators and community health workers to help guide next steps for patients and caregivers.
- Develop systems that make support services available to all cancer patients and survivors.
- Identify and address gaps in access to non-clinical support services for underserved populations.
- Adopt distress/symptom assessment tools and workflow models that identify the physical, social, psychological, and spiritual needs of patients throughout their cancer treatment.
- Support initiatives that address patient adherence to their cancer treatment plan.
- Establish a plan to provide equitable access to cancer treatment during public health emergencies.
Strategy E: Reduce cancer care costs incurred by patients and families.
Action Steps
- Support the implementation of evidence-based policy and systems change to reduce financial barriers to cancer care and unanticipated medical expenses.
- Encourage financial navigators to inform patients before a surgery/admission/procedure to let them know upfront costs and minimize surprise medical bills.
- Increase reimbursement rates under Medicaid.
- Increase insurance coverage and availability of financial navigators, patient navigators, and other support services.
- Increase the number of residents with comprehensive health insurance coverage.
- Ensure protections for preexisting conditions are maintained.
- Ensure protection against lifetime limits are maintained.
- Educate policymakers on the impact of financial stress on cancer care outcomes.
- Reduce out of pocket costs supporting cancer treatment and associated expenses.
- Increase the availability and insurance coverage of cancer rehabilitation services in communities.
Priority 2: Increase availability and access to palliative care early and throughout treatment.
Strategy A: Reduce barriers to quality palliative care.
Action Steps
- Increase the number of qualified palliative care providers.
- Establish a palliative care advisory council in Wisconsin.
- Increase insurance coverage of palliative care conversations, consultations, and services.
- Increase access to evidence-based interventions for cancer pain management, palliative care, and wellness.
- Develop culturally and linguistically appropriate tools that make it simpler for patients and families to request palliative care consultations.
- Provide the patient and family multiple opportunities and tools for initiating conversations related to palliative care throughout treatment.
- Promote additional training and certification for other providers and allied staff in palliative care.
- Promote additional training for physicians in cancer symptom management and palliative care throughout treatment, not just at the end of life.
- Educate providers, patients, and caregivers that palliative care is also available for symptom relief during treatment, not just end-of-life.
- Increase the number of palliative care fellows.
- Promote palliative care rotations with physicians in training and non-physicians, such as nurse practitioners and physician assistants
- Increase access to quality and secure telehealth services for palliative care.
- Establish a plan to provide equitable access to palliative care during public health emergencies.
Strategy B: Increase public, patient, and provider awareness of the benefits of introducing palliative care early in treatment.
Action Steps
- Create a public awareness campaign to inform the public on the benefits of palliative care, emphasizing its importance beyond end-of-life care.
- Educate non-curative cancer patients early in their treatment about palliative care and its role in their treatment.
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients.
- Educate the entire clinic team on palliative care and its benefits in cancer care.
- Work with communities and community health workers to provide culturally and linguistically appropriate palliative care information to the public, patients, and families.
- Advise cancer patients that quality end-of-life care is an expected part of cancer care.
- Advise cancer patients that palliative care during treatment is an option and part of cancer care.
- Advertise continuing education opportunities for health care providers in pain management or palliative care.
- Promote additional training for health care providers in cancer symptom management and palliative care.
Strategy C: Increase provider use of palliative care guidelines and quality standards.
Action Steps
- Follow clinical guidelines and create systems/workflows to identify patients who could benefit from palliative care consultation.
- Create electronic health record algorithms for the delivery of palliative care standards.
- Develop provider incentives for compliance with the American Society of Clinical Oncology (ASCO), American Academy of Hospice and Palliative Medicine (AAHPM), and National Comprehensive Cancer Network (NCCN) standards.
- Develop statewide publicly reported metrics for provider adherence to palliative care standards.
- Educate health care providers on evidence-based, best practices in palliative care.
- Train health care providers and support service professionals on how to conduct culturally and linguistically appropriate palliative care conversations between cancer patients and their families.
- Collect data on the use of palliative care during treatment and compliance with standards.
Priority 3: Increase patient and caregiver access to non-clinical support services, including care coordination, patient navigation, psychosocial support, and rehabilitation services.
Strategy A: Increase insurance coverage for non-clinical support services for survivors and caregivers.
Action Steps
- Review and summarize evidence on the health and financial benefits of non-clinical support services, including the return on investment (ROI) for the health care system.
- Conduct a cost-analysis of non-clinical support services.
- Educate policymakers on the needs for and benefits of non-clinical support services.
- Educate employers (including human resource professionals) and health care providers on the resources on state and federal legal protections, such as FMLA, for pediatric and adult cancer caregivers and survivors.
- Educate health insurance companies on the needs for and benefits of non-clinical support services.
- Educate leaders by framing cancer as a chronic disease, with rehabilitation models utilized for other chronic disease rehabilitation to instill the need for policy reform and funding.
- Increase insurance coverage and availability of financial navigators, patient navigators, and other support services.
- Encourage employers and cancer community stakeholders to provide and inform employees of any employer-specific provided benefits that may be provided to cancer survivors and caregivers.
Strategy B: Increase the availability of non-clinical support services for survivors and caregivers.
Action Steps
- Develop systems that make support and care coordination services available to all cancer patients and survivors.
- Utilize patient navigators to help patients and caregivers access support services and care coordination.
- Work with communities to develop and implement culturally and linguistically appropriate resources for patients and families.
- Identify and address gaps in access to non-clinical support services for underserved populations.
- Adopt distress/symptom assessment tools and workflow models that identify the physical, social, psychological, and spiritual needs of patients throughout their cancer treatment.
- Establish a plan to provide equitable access to non-clinical support services for survivors and caregivers during public health emergencies.
- Increase access to support programs/resources to assist the whole family throughout the cancer journey, including physical, social, spiritual and emotional support services, including resources tailored for children, adolescent and young adults, and adults with cancer.
- Increase support available to pediatric cancer survivors through school including Individualized Education Programs (IEP), educational consultants, 504 plans, and other relevant programs and resources.
Priority 4: Increase participation in clinical trials.
Strategy A: Increase access and availability of cancer clinical trials.
Action Steps
- Employ community health workers to help patients and their families to identify potential clinical trials.
- Work with communities to develop culturally and linguistically appropriate tools and resources to increase participation in cancer clinical trials.
- Train survivors as peer educators to increase participation in cancer clinical trials.
- Develop and implement public education campaigns to promote cancer clinical trials.
- Monitor federal legislation regarding funding for cancer clinical trials.
- Educate policymakers on the benefits of funding cancer clinical trials.
- Showcase how local and regional cancer centers are collaborating locally and participating in research efforts nationally.
- Encourage local and statewide foundations or cancer-related industry to fund cancer clinical trials.
- Maintain the state law that requires insurance companies to cover the costs of standard cancer care within the context of a clinical trial.
- Develop resources for patients and providers on cancer clinical trials and health insurance.
- Identify and address barriers to clinical trial participation such as fear, cultural beliefs, and potential medical and non-medical expenses.
- Increase public and private insurance coverage of medical and non-medical expenses incurred by participating in cancer clinical trials.
- Utilize technology to reduce transportation barriers to accessing cancer clinical trials.
- Establish transportation solutions to participate in cancer clinical trials.
- Establish a plan to provide equitable access to cancer clinical trials during public health emergencies.
Strategy B: Increase recruitment and inclusion of populations traditionally underrepresented in clinical trials.
Action Steps
- Identify and promote evidence-based strategies to increase utilization and accrual of patients to clinical trials in cancer care facilities.
- Establish benchmarks for the recruitment of each underrepresented population.
- Employ community health workers to support patients’ comprehensive understanding and informed decision-making in regards to cancer clinical trials.
- Work with communities to develop culturally and linguistically appropriate tools and resources to increase trust and acceptance of cancer clinical trials.
- Promote training opportunities for health care providers on the importance and availability of cancer clinical trials.
- Develop and implement provider reminder systems that identify patients who are potentially eligible for clinical trials.
- Develop and test clinical trial consent forms using principles of health literacy.
Priority 5: Increase the number of advance care planning conversations for all cancer patients early in their treatment.
Strategy A: Increase awareness of the importance of advance care planning.
Action Steps
- Develop best practice clinic workflow models to ensure advance care planning conversations are part of adult primary care and part of regularly reviewed patient health history.
- Increase public awareness about the importance of advance care planning conversations.
- Work with communities to develop and disseminate culturally and linguistically appropriate tools and models to increase awareness of the importance of advance care planning.
- Educate the entire clinic team on palliative care and its benefits in cancer care.
- Provide patient and family education on the importance of advanced care planning.
- Provide culturally and linguistically appropriate resources on advanced care planning for providers, cancer patients, and their families.
Strategy B: Improve accessibility of advance care planning documents within and across health systems.
Action Steps
- Establish statewide systems and solutions to increase the accessibility of advance care planning documents, such as an advance care planning registry and personal cards referencing advance care documents.
- Ensure that advance care planning documents are consistently and reliably stored in electronic health records and accessible within and across medical settings.
- Promote access to and utilization of quality state-approved advanced care documents.
- Support efforts to improve electronic health records and patient charts to include easy access to advance care planning documents for providers and patients.
- Employ community health workers to encourage and assist patients in completing advance care planning documents.
- Provide the patient and family multiple opportunities and tools for initiating conversations related to advance care planning.
- Provide patient and family education on the importance of advanced directives and how to ask for them.
Strategy C: Create health system strategies to routinely assess and review advance care plans throughout the cancer experience, including diagnosis, treatment, survivorship, and end of life.
Action Steps
- Facilitate advanced care planning conversations with all cancer patients to review or develop an advance care plan early in their treatment.
- Develop models or algorithms for reviewing patient advance care plans throughout the cancer experience.
- Develop uniform system-wide methods for making quality advanced care documents readily available.
- Integrate advance care planning into survivorship services at the beginning of treatment.
- Educate cancer providers and the community that advance care planning is an opportunity to empower cancer patients in setting goals of care.
- Employ community health workers to encourage and assist patients in completing advance care planning documents.
- Work with communities to develop and disseminate culturally and linguistically appropriate tools and models for the facilitation of advance care planning conversations.
- Educate providers on the need for and the reimbursement of advanced directives conversations.
- Collect data and quality measures at the health care system level about the number of advance care planning conversations and patient/family satisfaction with conversations.
Chapter 4 Plan Measures
Priority 1: Increase availability and access to quality cancer care.
Priority 2: Increase availability and access to palliative care early and throughout treatment.
Priority 3: Increase patient and caregiver access to non-clinical support services, including care coordination, patient navigation, psychosocial support, and rehabilitation services.
Priority 4: Increase participation in clinical trials.
Chapter 5
Survivorship
Chapter 5 Overview

Select a priority to learn more
- Priority 1 Increase awareness of issues relevant to cancer survivors and caregivers.
- Priority 2 Increase the implementation of best practices for the transition from active treatment to post-treatment care.
- Priority 3 Increase provider, patient, and caregiver awareness of the importance of cancer risk reduction behaviors and cancer screening for cancer survivors.
More people in Wisconsin, and the nation, are surviving cancer.
In 2019, almost 300,000 Wisconsinites were living with a cancer diagnosis.1 This number is expected to grow by tens of thousands every year, as advancements occur for early detection and treatment, and as the population grows and ages.
In 2019, 67 percent of US cancer survivors (10.3 million people) had survived five or more years after their diagnosis.2 More than 16.9 million Americans with a history of cancer were alive, with many more projected to survive in the near future.3
Cancer survivors regularly report unique challenges, health issues, and quality-of-life concerns long after treatment ends. We can respond to the diverse needs of Wisconsin’s growing survivor population by addressing cancer survivorship issues across the cancer care continuum.
How we define “cancer survivorship”
According to the National Cancer Institute (NCI), “an individual is considered a cancer survivor from the time of diagnosis, through the balance of their life.”4 Survivors include those with a current diagnosis and those now free from cancer. Caregivers (often called “co-survivors”), family members, and friends are an important part of the survivor experience.
Cancer survivorship refers to “the health and life of a person with a cancer, post-treatment until the end of life.” 4 Cancer survivorship issues can include:
- The long-term physical, mental, emotional, social, and financial effects of cancer
- The ability to access health care and follow-up treatment
- The transition from active cancer treatment to post-treatment primary care
- The effects of cancer that are late to emerge
- The risk of subsequent cancers
- Quality of life and well-being
The Takeaway
Cancer should be considered a chronic disease with long-term risks, adverse health impacts, and unique quality-of-life concerns that may last throughout a person’s lifetime. Special effort should be taken to educate providers about survivorship needs. To reduce the burden of subsequent cancers among survivors, we should focus attention on risk reduction, prevention, and screening strategies within this population.
Together, we can improve the long-term quality of life for Wisconsin’s growing number of cancer survivors.
Key Terms
Cancer survivor: An individual is considered a cancer survivor from the time of diagnosis, through the balance of his or her life.4 Survivors include those with a current diagnosis and those now free from cancer.
Caregiver: A person who gives care to someone living with a cancer diagnosis. Caregivers may be family members, friends, health professionals, social workers, or members of the clergy. They may give care at home or in a hospital or other health care setting or from afar.5
Co-survivor: The persons who support cancer survivors and who are affected by their diagnosis, including family members, friends, colleagues, and caregivers.
Survivorship care plan: A detailed plan given to a patient after treatment ends that contains a summary of the patient’s treatment, along with recommendations for follow-up care.6
References:
- National Cancer Institute. (2019). State Cancer Profiles: Wisconsin. Retrieved from: https://statecancerprofiles.cancer.gov/quick-profiles/index.php?statename=wisconsin#t=3
- Bluethmann SM, Mariotto AB, Rowland, JH. Anticipating the “Silver Tsunami”: Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016; 25:1029-1036.
- Miller, K. D., Nogueira, L., Mariotto, A. B., Rowland, J. H., Yabroff, K. R., Alfano, C. M., … & Siegel, R. L. (2019). Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin, 69(5), 363-385.
- National Cancer Institute. (2020). Office of Cancer Survivorship. Retrieved from Statistics, Graphs and Definitions: https://cancercontrol.cancer.gov/ocs/statistics/index.html#definition-survivorship
- National Cancer Institute. (2020, January 3). Coping with Cancer. Retrieved from Support for Caregivers of Cancer Patients: https://www.cancer.gov/about-cancer/coping/caregiver-support
- National Cancer Institute. (2019, October 4). Survivorship. Retrieved from Follow-Up Medical Care: https://www.cancer.gov/about-cancer/coping/survivorship/follow-up-care
Priority 1: Increase awareness of issues relevant to cancer survivors and caregivers.
Strategy A: Increase collection and dissemination of data identifying the unique needs of cancer survivors and caregivers.
Action Steps
- Acknowledge the growing needs of the increasing number of cancer survivors in Wisconsin.
- Measure and report on cancer survivors’ statistics regularly, including prevalence, late effects of treatment, and quality of life.
- Routinely collect state and region-specific information from cancer survivors and caregivers to understand and address their unique needs.
- Create and disseminate routine reports documenting the cancer survivor population, trends, and the unique needs of both survivors and caregivers.
- Incorporate data on cancer survivors in conversations about cancer incidence and mortality.
- Identify and measure disparities in cancer survival rates and quality-of-life measures.
- Track utilization of non-clinical support services by survivors and their caregivers.
- Assess gaps in access and use of non-clinical support services for underserved populations.
- Promote research to improve the quality of life for survivors that addresses the physical, cognitive, social, psychological, and spiritual impacts of treatment from diagnosis through late effects.
Strategy B: Inform providers and the public of the unique issues relevant to cancer survivors and caregivers.
Action Steps
- Educate health care providers on the physical, social, psychological, and spiritual dimensions of cancer survivorship.
- Educate provider organizations on how to assist survivors in addressing survivorship issues.
- Develop educational tools to publicize the unique and ongoing challenges of cancer survivorship.
- Educate policymakers on survivorship issues.
- Encourage survivors to share their stories with their communities.
- Gather and incorporate the survivor perspective into risk reduction messaging and activities.
- Educate school administrators, teachers, and the support staff on the needs of children with cancer during and after cancer treatment.
- Include patient and cancer survivor representation and input in research projects.
- Educate employers on the needs of cancer survivors and caregivers.
- Create an awareness campaign on the unique needs of cancer survivors and caregivers.
- Increase awareness of the lifetime impact of cancer on survivors and families, including pediatric and adolescent and young adult survivors.
Priority 2: Increase the implementation of best practices for the transition from active treatment to post-treatment care.
Strategy A: Increase utilization and effectiveness of survivorship care programs.
Action Steps
- Increase insurance coverage for survivorship services from the clinic and support staff.
- Employ patient navigators and community health workers to help patients and caregivers access survivorship services.
- Train survivors and caregivers on shared decision-making and strategies for being actively involved in care decisions.
- Develop models of care for rehabilitation and wellness services.
- Increase knowledge and availability of survivorship resources, such as rehabilitation services, physiological, and caregiver support.
- Include fertility planning discussions before, during, and after treatment for certain cancers.
- Include long-term risks of treatment (including second cancers) in discussions before, during, and after treatment for certain cancers.
- Incorporate evidence-based complementary and alternative therapies into survivorship care programs.
- Fund and conduct research projects to measure the effectiveness of non-clinical approaches on cancer survivor quality of life.
- Provide individualized survivor care plans to survivors with information specific to their treatment and ongoing health.
- Adapt chronic disease self-management programs for cancer survivors.
- Develop culturally and linguistically appropriate support services based on community-identified strengths and needs.
Strategy B: Establish health systems-level quality improvement metrics and processes to improve transitions from active treatment to post-treatment care.
Action Steps
- Encourage health care systems to invest in the integration of cancer survivor services and the transition to primary care.
- Educate insurance companies about the benefits of paying for the integration of cancer survivor services and the transition to primary care treatment.
- Provide individualized survivor care plans to survivors with information specific to their treatment and ongoing health needs.
- Provide individualized survivor care plans to the survivor’s primary care team with information specific to the survivor’s treatment and ongoing health needs.
- Implement collaborative care models for the management of distress and/or psychiatric disorders.
- Establish collaborative care in the treatment and survivorship team, including mental health professionals and the cross-training of medical professionals.
- Increase state-level surveillance of cancer survivors.
- Assess gaps in access and use of non-clinical support services for underserved populations.
- Develop and implement guidelines for access to survivorship care for pediatric cancer survivors, such as the Children’s Oncology Group Passport to Care.
Strategy C: Increase community-clinical linkages to community support services.
Action Steps
- Increase provider access and referral to survivorship resources within organizations and in the community.
- Work with communities to develop and/or promote culturally and linguistically appropriate support services.
- Assess and increase the availability and use of cancer rehabilitation and wellness services in communities.
- Create community- or region-wide partnerships to leverage and share survivorship resources across organizations.
- Work with communities to identify non-traditional solutions that provide survivors with non-medical support.
- Link survivors with organizations that promote and deliver training for the active patient model.
- Develop culturally and linguistically appropriate support services based on community-identified strengths and needs.
- Identify and address health inequities in survivor populations.
- Assess gaps in access and use of non-clinical support services for underserved populations.
Establish a plan to provide equitable access to community support services for survivors and caregivers during public health emergencies.
Priority 3: Increase provider, patient, and caregiver awareness of the importance of cancer risk reduction behaviors and cancer screening for cancer survivors.
Strategy A: Tailor cancer risk reduction messages and activities to meet the unique needs of cancer survivors.
Action Steps
- Educate survivors on the importance of regular check-ups with their primary care provider for overall health.
- Educate survivors and caregivers on maintaining a healthy lifestyle as a way to decrease the risk of cancer recurrence and side effects from treatment.
- Educate primary care teams on the increased importance of risk reduction behaviors.
- Implement tailored approaches to increase risk reduction behaviors among cancer survivors.
- Utilize patient navigators and community health workers to help patients and caregivers access survivorship risk reduction services and resources.
- Increase provider access and referral to survivorship resources within organizations and in the community.
- Encourage survivors to regularly participate in physical activity in safe and empowering ways.
- Fully fund a Wisconsin comprehensive tobacco prevention and control program consistent with CDC funding recommendations that address tobacco use and cessation in cancer survivors.
- Support workplace policies to prevent and reduce excessive drinking and programs that emphasize the importance of healthy eating during and after cancer treatment.
Strategy B: Tailor cancer screening messages and activities to meet the unique needs of cancer survivors.
Action Steps
- Educate survivors about their potential risk for secondary cancers due to treatment exposures.
- Educate survivors on when and how to get screened for cancers.
- Educate primary care teams on early detection guidelines among cancer survivors.
- Integrate risk assessment tools within primary care teams to provide tailored evidence-based screening recommendations to cancer survivors.
- Implement a tailored approach to increase the utilization of recommended cancer screenings among cancer survivors.
- Educate communities about risk factors that may change standard cancer screening recommendations.
- Utilize patient navigators and community health workers to help patients and caregivers access screening services and ask questions about their screening recommendations.
- Forecast screening activities in patient-accessed electronic health records.
- Provide individualized survivor care plans to survivors with information specific to their treatment and ongoing health.
Chapter 5 Plan Measures
Priority 2: Increase the implementation of best practices for the transition from active treatment to post-treatment care.
Priority 3: Increase provider, patient, and caregiver awareness of the importance of cancer risk reduction behaviors and cancer screening for cancer survivors.
Chapter 6
End of Life
Chapter 6 Overview

Select a priority to learn more
Cancer is a leading cause of death in Wisconsin.
Quality end-of-life care can reduce suffering and is an essential component of cancer care.
Conversations about potential end-of-life concerns should begin at the earliest possible stage after diagnosis. Advance care documents can give patients, providers, caregivers, and family members the opportunity to discuss the patient’s wishes, concerns, and goals of care.
For patients, caregivers, and families, end-of-life concerns can be physical, psychological, social, and spiritual. Additional training may be needed to help medical professionals better understand and respond to these concerns; such training should include strategies to support the emotional and mental health needs of health care providers engaged in end-of-life work.
The Takeaway
Everyone in Wisconsin deserves to approach the end of life with dignity. This can be achieved by increasing access to culturally competent end-of-life care, including palliative medicine and hospice. Likewise, health care providers deserve the training and mental health supports needed to assess and respond to the end-of-life concerns of patients and families.
Together, we can reduce suffering from cancer for patients and their loved ones.
Key Terms
Advance care planning: The process of deciding and sharing a person’s preferences about receiving health care if they later become unable to speak for themselves. These preferences are usually documented in documents called advance directives.2
Advance directives: Legal documents that states a person’s wishes about receiving medical care if that person is no longer able to make medical decisions because of a serious illness or injury. Advance directives also may give a person the authority to make medical decisions for another person when that person can no longer make decisions for themselves.3
Hospice: A program that gives special care to people who are near the end of life and have stopped treatment to cure or control their disease. Hospice offers physical, emotional, social, and spiritual support for patients and their families. The main goal of hospice care is to control pain and other symptoms of illness, so patients can be as comfortable and alert as possible. It is usually given at home, but may also be given in a hospice center, hospital, or nursing home.4
Palliative care: Care given to improve the quality of life of patients who have a serious or life-threatening disease. The goal of palliative care is to prevent or reduce the symptoms of a disease, side effects caused by treatment, and the psychological, social, and spiritual problems related to a disease or its treatment. Palliative care can begin at any time during treatment and can occur alongside curative treatment.5
References:
- National Hospice and Palliative Care Organization. (2017). Some Differences Between Palliative Care and Hospice. Retrieved from https://www.nia.nih.gov/health/what-are-palliative-care-and-hospice-care Published with permission of the National Hospice and Palliative Care Organization, all rights reserved. For a more complete chart please see: https://www.nhpco.org/wp-content/uploads/2019/04/PalliativeCare_VS_Hospice.pdf
- National Institutes of Health. (2018, January 15). National Institute on Aging. Retrieved from Advance Care Planning: Healthcare Directives: https://www.nia.nih.gov/health/advance-care-planning-healthcare-directives
- National Cancer Institute. (2015, March 10). Advance Directives. Retrieved from https://www.cancer.gov/about-cancer/managing-care/advance-directives
- National Cancer Institute. (2018, September 19). Choices for Care When Treatment May Not Be an Option. Retrieved from Hospice Care: https://www.cancer.gov/about-cancer/advanced-cancer/care-choices#HC
- National Cancer Institute. (2017, October 20). Palliative Care in Cancer. Retrieved from https://www.cancer.gov/about-cancer/advanced-cancer/care-choices/palliative-care-fact-sheet
Priority 1: Increase availability and access to palliative medicine during end-of-life care.
Strategy A: Reduce barriers to access quality palliative care.
Action Steps
- Inform providers, patients, and caregivers that palliative care is also available for symptom relief during treatment, not just end of life.
- Educate providers, patients, and caregivers that palliative care can occur in or out of hospice settings.
- Increase the number of qualified palliative care providers.
- Establish a palliative care advisory council in Wisconsin.
- Increase insurance coverage of palliative care conversations and services.
- Increase access to evidence-based interventions for cancer pain management, palliative care, and wellness.
- Promote additional training and certification for other providers and allied staff (nurses, LPNs, CNAs, etc.) in palliative care.
- Develop culturally and linguistically appropriate tools that make it simpler for patients and families to request palliative care consultations.
- Provide culturally and linguistically appropriate resources on end-of-life care for providers, cancer patients, and their families.
- Incorporate the cancer perspective while addressing widespread opioid abuse issues.
- Establish a plan to provide equitable access to palliative care during public health emergencies.
- Ensure access to pediatric palliative/hospice care programs and support hospice workers specifically trained in the unique needs of pediatric patients and their families.
Strategy B: Increase public, patient, and provider awareness of the benefits of palliative care at the end of life.
Action Steps
- Create a public awareness campaign to inform the public about the benefits of palliative care.
- Educate patients early in their treatment about palliative care and its role in their treatment.
- Educate providers, patients, and caregivers that palliative care can occur in or out of hospice settings.
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients.
- Educate the entire clinic team on palliative care and its benefits in cancer care.
- Work with communities and community health workers to provide culturally and linguistically appropriate palliative care information to the public, patients, and families.
- Promote access to and utilization of quality state-approved advanced care documents.
- Advise cancer patients that quality end-of-life care is an expected part of cancer care.
- Promote additional training for health care providers in cancer symptom management and palliative care.
- Advertise continuing education opportunities for health care providers in pain management or palliative care.
Strategy C: Increase provider use of palliative care guidelines and quality standards.
Action Steps
- Create electronic health record algorithms for the delivery of palliative care standards.
- Develop provider incentives for compliance with the American Society of Clinical Oncology (ASCO), American Academy of Hospice and Palliative Medicine (AAHPM), and National Comprehensive Cancer Network (NCCN) standards.
- Develop statewide publicly reported metrics for provider adherence to palliative care standards.
- Educate health care providers on evidence-based, best practices in palliative care.
- Train health care providers and other professions related to end-of-life care on how to conduct culturally and linguistically appropriate palliative care conversations between cancer patients and their families.
- Establish a palliative care advisory council in Wisconsin that determines metrics to measure the use of palliative care.
Priority 2: Increase access to quality end-of-life care.
Strategy A: Increase cancer patient referrals to and utilization of hospice services.
Action Steps
- Create a report card by county or region to measure the percentage of cancer patient referrals and length of stay in hospice.
- Work with communities to create and disseminate culturally and linguistically appropriate resources on end-of-life care for providers, cancer patients, and their families.
- Develop culturally and linguistically appropriate tools that make it simpler for patients and families to request palliative care consultations.
- Create and distribute a hospice toolkit that includes resources, forms, and regulations for hospice services.
- Promote the establishment of a health care power of attorney, living will, and end-of-life wishes early in diagnosis, so that the patient’s wishes will be known.
- Advise cancer patients that quality end-of-life care is an expected part of cancer care.
- Establish a plan to provide equitable access to quality end-of-life care during public health emergencies.
Strategy B: Decrease the number of cancer patients who die in intensive care units and emergency rooms.
Action Steps
- Establish baseline data on cancer patient intensive care unit and emergency room deaths.
- Provide training opportunities and guidelines for intensive care unit and emergency room staff on palliative care services and how to access them.
- Establish algorithms that the intensive care unit and emergency room staff can use to quickly identify appropriate cancer patients for palliative care consultation.
- Work with communities to create and disseminate culturally and linguistically appropriate resources on end-of-life care for providers, cancer patients, and their families.
- Educate health care teams on the importance of respecting and supporting decisions of the cancer patient and their family.
- Promote and provide culturally and linguistically appropriate bereavement services to patients and families.
Chapter 6 Plan Measures
Priority 1: Increase availability and access to palliative medicine during end-of-life care.
Priority 2: Increase access to quality end-of-life care.
Chapter 7
Data
Chapter 7 Overview
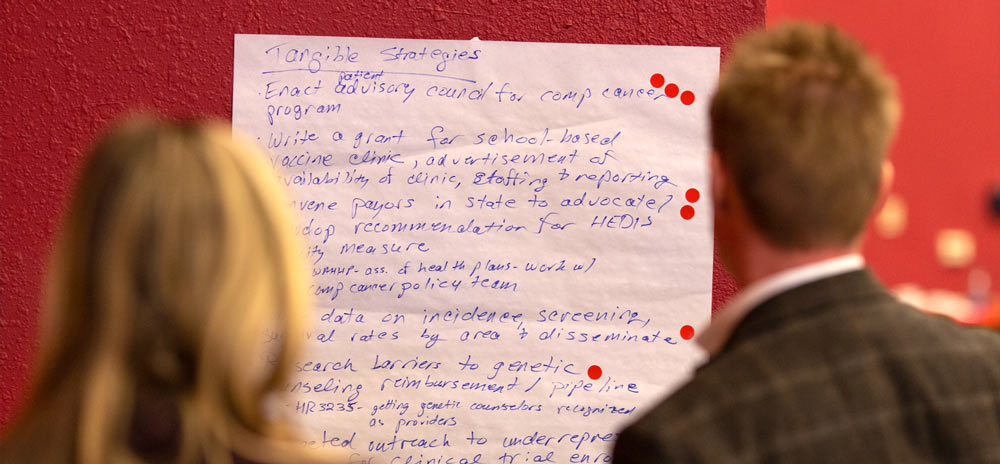
Select a priority to learn more
To understand the full burden and impact of cancer in Wisconsin, we need reliable, quality data.
Data helps us understand where to allocate our resources, where progress is made, and where we need additional work.
Wisconsin has robust public health data systems, including a Wisconsin population-based cancer registry (the Wisconsin Cancer Reporting System). Unfortunately, some populations within Wisconsin are underrepresented in the data that helps us identify differences in cancer risk and health outcomes. Areas for improvement exist in data collection, use of existing data, and increasing the linkages with other data systems.
Data opportunities in Wisconsin
Data drives the decisions, policies, strategies, and activities that work to collectively improve and prevent cancer outcomes in Wisconsin. To enhance cancer data in Wisconsin, several opportunities exist:
- Establish and maintain data agreements to report all cancer cases from Wisconsinites who receive care in Minnesota (or other nearby states).
- Improve the ability of health care systems to report underreported fields to produce more accurate estimations of cancer cases and mortality.
- Increase the number of certified tumor registrars and trained cancer reporters across Wisconsin, to improve timely data collection and dissemination.
The Takeaway
To better understand the impact of cancer in Wisconsin, we need to improve the ongoing, timely, and systematic collection and analysis of cancer and cancer risk data—especially data that reflect the outcomes and health status related to disparately impacted populations.
Key Terms
Behavioral Risk Factor Surveillance System (BRFSS): The nation’s system of health-related telephone surveys that collect state data about United States residents 18 years and older regarding their self-reported “health-related risk behaviors, chronic health conditions and use of preventive services.”1
Incidence: The number of new cases of a disease diagnosed each year.2
Mortality: In medicine, this term is used for death rate, or the number of deaths in a certain group of people in a certain period.3
SEER: The National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program provides information on cancer statistics in an effort to reduce the cancer burden among the US population.4
Wisconsin Cancer Reporting System (WCRS): The Wisconsin population-based cancer registry, which provides direct access to information about cancer incidence and mortality in Wisconsin.5
References:
-
- Centers for Disease Control and Prevention. (2019, November 5). Behavioral Risk Factor Surveillance System. Retrieved from https://www.cdc.gov/brfss/index.html
- National Cancer Institute. (n.d.). NCI Dictionary of Cancer Terms. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms
- National Cancer Institute. (n.d.). NCI Dictionary of Cancer Terms. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms
- National Cancer Institute. (n.d.). Surveillance, Epidemiology, and End Results Program. Retrieved from https://seer.cancer.gov/
- Wisconsin Cancer Reporting System (WCRS): Wisconsin Department of Health Services. (2019, February 12). Wisconsin Cancer Reporting System. Retrieved from https://www.dhs.wisconsin.gov/wcrs/index.htm
Priority 1: Promote awareness and use of the Wisconsin Cancer Reporting System’s data.
Strategy A: Support the Wisconsin Cancer Reporting System in its mission to provide accurate and timely data.
Action Steps
- Increase the number of Certified Tumor Registrars and trained cancer reporters, especially in rural facilities.
- Increase reporting from non-hospital facilities, such as pathology labs.
- Increase reporting from out of state facilities that diagnose and/or treat Wisconsin residents.
- Promote timely reporting by facilities to the Wisconsin Cancer Reporting System.
- Increase awareness of importance of reporting and capturing demographic information, specifically related to race, ethnicity and applicable social determinants of health.
- Improve the quality and completeness of cancer patient data reported to the Wisconsin Cancer Reporting System, particularly regarding the stage of disease at diagnosis and treatment.
- Train health care providers on the law and requirements for reporting cancer cases to the Wisconsin Cancer Reporting System.
- Link cancer-related data with relevant geographic information.
- Recognize facilities for compliance and quality submission.
Strategy B: Promote the use of cancer registry data.
Action Steps
- Promote the work of the Wisconsin Cancer Reporting System to ensure Wisconsin residents understand the need and benefits of the Wisconsin Cancer Reporting System.
- Increase awareness of publicly available cancer registry data.
- Establish a working group of Wisconsin cancer centers to increase availability and facilitate use of cancer data in research activities.
- Review administrative rules and help communicate the policies and procedures to data users.
- Promote existing cancer-related data and relevant reports.
- Provide policymakers with Wisconsin specific cancer-related data to inform policies and decision-making.
Priority 2: Improve Wisconsin-specific cancer-related data sources.
Strategy A: Improve data collection for existing data sources.
Action Steps
- Enhance data collection from additional sources to address gaps.
- Increase funding for data collection.
- Incorporate cancer-related issues into existing data collection systems.
- Facilitate a collaboration of cancer stakeholders to assess emerging cancer issues and incorporate them into existing data reporting systems.
- Engage underrepresented communities in identifying critical data gaps.
- Support initiatives that increase student trainee opportunities at the Wisconsin Cancer Reporting System.
Strategy B: Improve the comprehensiveness of data captured by existing sources.
Action Steps
- Collect information on the social determinants of health.
- Collaborate with other cancer-related stakeholders to help facilitate data linkages and to determine what further data should be captured.
- Establish a registry that tracks cancer screening completion.
- Assess cancer screening and cancer prevention efforts statewide and their impact on cancer incidence and mortality.
- Establish a collaborative resource of advance care planning documents.
- Enable interoperability among institutions and systems that support care delivery across the cancer care continuum, from prevention through treatment, survivorship, and end-of-life care.
- Collaborate with other researchers to identify gaps and possible solutions.
- Increase funding for data collection.
- Increase funding for Certified Tumor Registrars and trained cancer reporters.
Strategy C: Improve utilization and timeliness of existing data.
Action Steps
- Increase awareness about the availability of existing data.
- Increase the accessibility of existing data.
- Utilize existing data in dissemination products regarding cancer burdens and topics.
- Educate end-users on the utilization and interpretations of cancer findings.
- Tailor data findings and messages to multiple audiences and share what impact these findings may have.
- Explore existing data to identify areas for improvement and the highest need regarding screening, diagnosis, treatment, and survivorship.
- Link cancer-related data with relevant geographic information.
- Inventory and promote existing cancer-related data and relevant reports.
Priority 3: Monitor data related to emerging cancer issues.
Strategy A: Collect data to measure and identify emerging cancer needs in Wisconsin.
Action Steps
- Identify missing data and support efforts to collect missing data.
- Collaborate with other stakeholders to develop new cancer data-related projects and dissemination products.
- Measure and report on cancer survivor’s statistics given the growing survivor population.
- Capture demographic information while collecting data, specifically related to race and ethnicity.
- Identify and inventory environmental-related cancer risk data and relevant findings with experts on the issue.
- Expand the collection and availability of data on those disparately impacted by cancer.
- Identify data on the financial impacts of cancer including loss of income, out-of-pocket costs for care, financial hardship/medical bankruptcy, travel, and long-term financial impacts on the survivors such as employability and insurability, including pediatric and AYA survivors.
- Collect and report data on pediatric cancer in Wisconsin and identify disparities.
Strategy B: Identify and track existing and potential cancer disparities and burdens in Wisconsin.
Action Steps
- Inventory cancer risk data and relevant findings with experts on the related issue or cancer type.
- Link cancer-related data with relevant geographic information.
- Engage under-represented communities in identifying critical data gaps.
- Promote research that identifies and discusses cancer disparities and potential solutions that address the contributing factors of these disparities.
- Collaborate with other researchers to identify gaps and possible solutions.
- Increase accessibility of existing data.
- Report findings in a variety of ways to ensure accessibility to all stakeholders.
- Engage community-based research on the incidence and impact of cancer disparities in their communities.
- Assess rural-urban cancer rates in Wisconsin and develop and implement rural-focused cancer control strategies in areas with high rural cancer mortality rates.
- Identify and address the social determinants of health and their influence on cancer rates.
- Measure the impact public health emergencies have on cancer continuum services and cancer outcomes.
